Cancer: What is Glioblastoma Multiforme and Why is it Difficult to Treat
- Science Holic
- Sep 30, 2025
- 6 min read
Author: Eric Lin
Editors: Jonathan Chen, Miriam Heikal, Kacey Ye
Artist: Alvina Zheng

In America, cancer is second behind heart disease in leading causes of death. Among all types of cancers, brain cancers are one of the deadliest, with the most fatal and most common form of brain cancer being Glioblastoma Multiforme(GBM). GBM is classified as a grade 4 brain tumor arising from supportive tissue called astrocytes. Astrocytes in a normal brain are supportive tissue that help protect and support neurons in the brain. GBM’s classification as a grade 4 cancer indicates it is fast-growing and extremely aggressive. Currently, the causes of GBM are unknown, but family history could be a factor in getting GBM. In addition, the 5-year survival rate for GBM is very low, meaning less than 5% of patients with GBM survive 5 years after diagnosis. Compared to other cancers like breast and pancreatic cancers, GBM’s low survival rate is especially noticeable, with the median patient only surviving between 12 to 15 months.

The current standard treatment for GBM involves surgery in which as much of the tumor is removed as possible, and is followed by daily radiation and oral chemotherapy for six and a half weeks, then a six-month regimen of oral chemotherapy given five days a month. A chemotherapy drug called temozolomide is also commonly used for GBMs and slows tumor growth. While the current treatment for GBM is effective and has allowed people to live a few years longer, it is not curative, as it does not kill every tumor cell, and recurrence is common. This is due to three main factors: GBM’s intratumoral heterogeneity, its infiltrative nature, and biological barriers, such as the Blood-Brain Barrier (BBB). GBM’s intratumoral heterogeneity refers to the diverse subpopulations of cancer cells within each tumor. This means within each tumor there is a diverse population of cancer cells, each with potentially different mutations, genetic makeup, and even resistance to treatment. GBM’s infiltrative nature refers to the spread of the cancer. Malignant GBM cancer cells are known to spread quickly to other areas of the brain. Due to its fast spread, it is virtually impossible to completely remove GBM through surgery. Remaining GBM cells can quickly multiply, leading to recurrence of GBM. Finally, the blood-brain barrier is a biological wall that blocks most treatments from reaching GBM tumors in an effective concentration. In a normal brain, the blood-brain barrier is a semipermeable biological wall that helps filter pathogens and toxins from entering the brain. However, in patients with GBM, the blood-brain barrier impedes treatment agents, such as temozolomide, from reaching the tumor. All these factors contribute to GBM’s low survival rate and its being aggressive, hard to treat, and deadly.
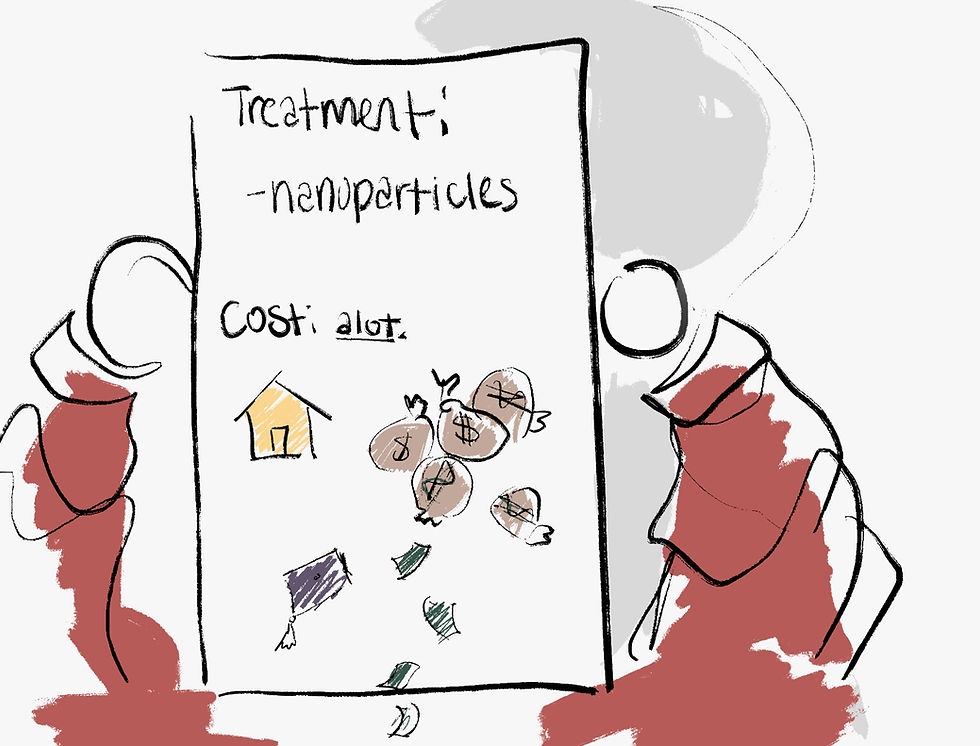
That said, research is being done to find ways to combat the difficulties found in standard GBM treatment to hopefully improve the odds of survival. One such method being tested right now is nanoparticle drug delivery systems. Nanoparticle drug delivery systems are a delivery system for medicine using nanoparticles, which are particles typically 10-20 nm in size, that can be modified to house medications. Nanoparticles can be easily engineered to cross the blood-brain barrier and carry multiple treatments that can help overcome challenges imposed by standard treatment. Due to their small size, being thousands of times smaller than a red blood cell, they slip through the blood-brain barrier and reach tumor sites. In addition, they can be modified with ligands, or molecules that latch onto certain proteins found on receptors on the surface of GBM tumors. They can also house gene silencing siRNA, analogous to jamming devices that disrupt the function of certain DNA strands. Think of them like a piece of malware that destroys genetic code (DNA) that promotes the cancer’s growth. By silencing these DNA strands, the spread of GBM can be reduced or completely stopped. Products like AGulX and Nanotherm are currently being tested in GBM treatment, with early trials showing promising results of increased survival times and reduction of GBM tumor sites. That said, nanoparticles face their own limitations. Nanoparticles are extremely expensive to produce and test, costing hundreds of thousands for a single nanoparticle. In addition, their efficacy results in early human trials have been modest, only adding a few months to the median survival time. That said, it's still an emerging field, and we have yet to see nanoparticles’ full potential in treating GBM.
In conclusion, GBM is one of the most common and aggressive forms of brain cancer. Multiple factors about GBM make it difficult to treat, leading to its poor survival rate. Emerging treatments like nanoparticle drug delivery systems have been shown as a promising avenue for future GBM treatment, but are hampered by the manufacturing and research costs. Hopefully, with future advancements in treatment plans, GBM’s survival rate may improve.
Citations:
Biau, J., Durando, X., Boux, F., Molnar, I., Moreau, J., Leyrat, B., Guillemin, F., Lavielle, A.,
Cremillieux, Y., Seddik, K., Dufort, S., De Beaumont, O., Thivat, E., & Duc, G. L. (2024a).
NANO-GBM trial of AGuIX nanoparticles with radiotherapy and temozolomide in the
treatment of newly diagnosed Glioblastoma: Phase 1b outcomes and MRI-based biodistribution.
Clinical and Translational Radiation Oncology, 48, 100833.
Biau, J., Durando, X., Boux, F., Molnar, I., Moreau, J., Leyrat, B., Guillemin, F., Lavielle, A.,
Cremillieux, Y., Seddik, K., Dufort, S., De Beaumont, O., Thivat, E., & Duc, G. L. (2024b).
NANO-GBM trial of AGuIX nanoparticles with radiotherapy and temozolomide in the
treatment of newly diagnosed Glioblastoma: Phase 1b outcomes and MRI-based biodistribution.
Clinical and Translational Radiation Oncology, 48, 100833.
Faris, J. (2025, March 4). Glioblastoma (GBM) - American Brain Tumor Association | Learn more.
American Brain Tumor Association. https://www.abta.org/tumor_types/glioblastoma-gbm/
Glioblastoma multiforme (GBM): advancing treatment for a dangerous brain tumor. (2023, October
30). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-
Glioblastoma multiformes (GBMs) | Boston Children’s Hospital. (n.d.).
Global Coalition for Adaptive Research. (2024, November 6). GBM AGILE | Glioblastoma Treatment
Adaptive Platform Trial. https://www.gcaresearch.org/research/gbm-agile/
Gregory, J. V., Kadiyala, P., Doherty, R., Cadena, M., Habeel, S., Ruoslahti, E., Lowenstein, P. R.,
Castro, M. G., & Lahann, J. (2020). Systemic brain tumor delivery of synthetic protein
nanoparticles for glioblastoma therapy. Nature Communications, 11(1).
Hersh, A. M., Alomari, S., & Tyler, B. M. (2022a). Crossing the Blood-Brain Barrier: Advances in
nanoparticle technology for drug delivery in Neuro-Oncology. International Journal of
Molecular Sciences, 23(8), 4153. https://doi.org/10.3390/ijms23084153
Hersh, A. M., Alomari, S., & Tyler, B. M. (2022b). Crossing the Blood-Brain Barrier: Advances in
nanoparticle technology for drug delivery in Neuro-Oncology. International Journal of
Molecular Sciences, 23(8), 4153. https://doi.org/10.3390/ijms23084153
Kumthekar, P., Ko, C. H., Paunesku, T., Dixit, K., Sonabend, A. M., Bloch, O., Tate, M., Schwartz,
M., Zuckerman, L., Lezon, R., Lukas, R. V., Jovanovic, B., McCortney, K., Colman, H., Chen,
S., Lai, B., Antipova, O., Deng, J., Li, L., . . . Stegh, A. H. (2021a). A first-in-human phase 0
clinical study of RNA interference–based spherical nucleic acids in patients with recurrent
glioblastoma. Science Translational Medicine, 13(584).
Kumthekar, P., Ko, C. H., Paunesku, T., Dixit, K., Sonabend, A. M., Bloch, O., Tate, M., Schwartz,
M., Zuckerman, L., Lezon, R., Lukas, R. V., Jovanovic, B., McCortney, K., Colman, H., Chen,
S., Lai, B., Antipova, O., Deng, J., Li, L., . . . Stegh, A. H. (2021b). A first-in-human phase 0
clinical study of RNA interference–based spherical nucleic acids in patients with recurrent
glioblastoma. Science Translational Medicine, 13(584).
Liu, D., Dai, X., Tao, Z., Zhou, H., Hong, W., Qian, H., Cheng, H., & Wang, X. (2023). Advances in
blood–brain barrier-crossing nanomedicine for anti-glioma. Cancer Nanotechnology, 14(1).
Maier-Hauff, K., Rothe, R., Scholz, R., Gneveckow, U., Wust, P., Thiesen, B., Feussner, A., Von
Deimling, A., Waldoefner, N., Felix, R., & Jordan, A. (2006a). Intracranial Thermotherapy
using Magnetic Nanoparticles Combined with External Beam Radiotherapy: Results of a
Feasibility Study on Patients with Glioblastoma Multiforme. Journal of Neuro-Oncology, 81(1),
Maier-Hauff, K., Rothe, R., Scholz, R., Gneveckow, U., Wust, P., Thiesen, B., Feussner, A., Von
Deimling, A., Waldoefner, N., Felix, R., & Jordan, A. (2006b). Intracranial Thermotherapy
using Magnetic Nanoparticles Combined with External Beam Radiotherapy: Results of a
Feasibility Study on Patients with Glioblastoma Multiforme. Journal of Neuro-Oncology, 81(1),
Paradise, J. (2019). Regulating nanomedicine at the Food and Drug Administration. The AMA
Journal of Ethic, 21(4), E347-355. https://doi.org/10.1001/amajethics.2019.347
Sa, N. T. (2024, May 30). NH TherAguix receives FDA Fast Track designation. GlobeNewswire
News Room. https://www.globenewswire.com/news-release/2024/05/30/2890749/0/en/NH-
Seker-Polat, F., Degirmenci, N. P., Solaroglu, I., & Bagci-Onder, T. (2022). Tumor Cell Infiltration
into the Brain in Glioblastoma: From Mechanisms to Clinical Perspectives. Cancers, 14(2), 443.
Sottoriva, A., Spiteri, I., Piccirillo, S. G. M., Touloumis, A., Collins, V. P., Marioni, J. C., Curtis, C.,
Watts, C., & Tavaré, S. (2013). Intratumor heterogeneity in human glioblastoma reflects cancer
evolutionary dynamics. Proceedings of the National Academy of Sciences, 110(10), 4009–4014.
Wu, J. (2021). The Enhanced Permeability and Retention (EPR) effect: the significance of the
concept and methods to enhance its application. Journal of Personalized Medicine, 11(8), 771.
Saraiva, C., Praça, C., Ferreira, R., Santos, T., Ferreira, L., & Bernardino, L. (2016). Nanoparticle-
mediated brain drug delivery: Overcoming blood–brain barrier to treat neurodegenerative
diseases. Journal of Controlled Release, 235, 34–47.
Gacche, R. N., & Assaraf, Y. G. (2018). Redundant angiogenic signaling and tumor drug resistance.
Drug Resistance Updates, 36, 47–76. https://doi.org/10.1016/j.drup.2018.01.002
Ahmed, M., Canney, M., Carpentier, A., & Idbaih, A. (2023). Overcoming the blood brain barrier in
glioblastoma: Status and future perspective. Revue Neurologique, 179(5), 430–436.



Comments