Healing with Polymers: How Bioengineered Materials Are Transforming Orthopedic Medicine
- Science Holic
- Aug 6, 2025
- 6 min read
Author: Joshua Payne
Editors: Fiona Cheng, Oscar Chen, Jonathan Chen
Artist: Helen Gong

Bones are living structures that comprise the framework of our bodies by providing structural support, enabling movement, and protecting vital organs that keep us alive. But bones are not invincible; age, poor lifestyle habits, illness, or unforeseen accidents will weaken or destroy even the strongest skeletons. In 2019, there were an estimated 178 million new bone fractures worldwide and 455 million people living with either short-term or long-term symptoms from fractures.
According to the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) in 2019, researchers derived these figures by comparing the “rates of global incidence, prevalence, and years lived with disability” caused by fractures across the 21 GBD regions and 204 countries and territories. Injuries can cause an inability to work, decreased productivity, disability, impaired quality of life, health loss, and high health-care costs. This would place a significant burden on individuals, families, societies, and health-care systems” (GBD 2019 Fracture Collaborators e580).
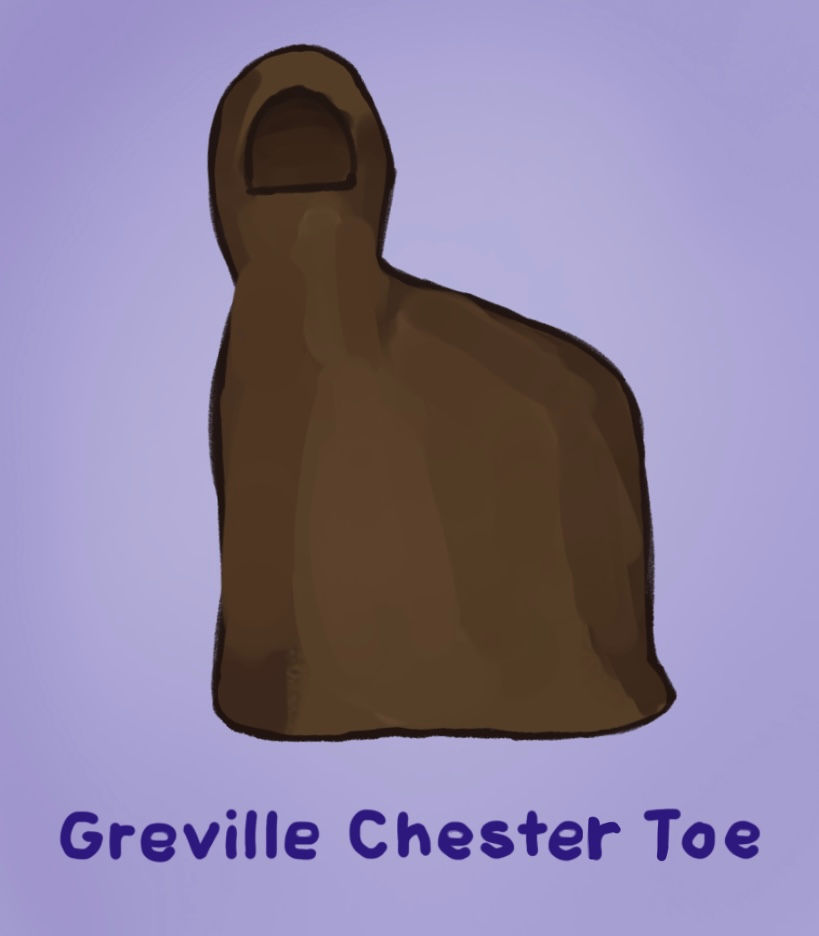
Since ancient times, people have created prosthetics in an attempt to overcome the debilitating consequences of injury and even amputation. In order to truly understand how far innovations in prosthetics and orthopedic medicine have come, it is essential to explore how prosthetic and implant technologies have evolved over the millennia, from crude wooden substitutes to revolutionary biocompatible and bioresorbable systems. The two earliest known prosthetics, dating back to around the same period, originated from ancient Egypt. The Greville Chester toe, believed to be between 2,600 and 3,400 years old, was made from cartonnage, a type of inflexible “papier-mâché made from glue, linen, and plaster.” This makeup led researchers to surmise that the prosthetic served cosmetic purposes only (MedlinePlus 20). In contrast, the Cairo toe, a flexible wooden and leather prosthetic toe, estimated to be between 2,700 and 3,000 years old, was often “refitted for the wearer”. Because of these characteristics, the Cario toe is thought to be the “earliest known practical artificial limb”. Later in 300 B.C. in Italy, an ancient Roman nobleman used the Capula leg which is a “bronze and hollowed-out wood prosthetic leg held up with leather straps” (Medline Plus 21).
War caused numerous soldiers to lose their limbs, bringing forth a dire need for artificial limbs. In 200 B.C., Roman general Marcus Sergius Silus lost his right hand during the Second Punic War, replacing it with an iron version designed to hold his shield. Additionally, knights in the Middle Ages sometimes used wooden limbs for either battle or riding horses (Medline Plus 21). In the 16th century, French surgeon Ambroise Paré designed some of the first functional prosthetics for soldiers returning from the battlefield. A record-breaking 60,000 amputations were performed during the bloody battles of the American Civil War, accounting for approximately 75% of the 80,000 surgeries administered to wounded soldiers ("Medical Inventions: American Civil War" 0:50). As a result, the overwhelming demand for prosthetic limbs led to the development of more sophisticated inventions, causing the number of patents for prosthetics to almost quadruple. One of the most notable patents was the Hanger Limb, the first prosthetic leg to have a rubber ankle and cushioned heel which significantly reduced the discomfort amputees had to endure (MedlinePlus 21).
Prosthetics were still primarily made from wood, metal, glue, and leather up to the 20th century, but they became significantly more functional. Between the 5th and 8th centuries, functional artificial feet were crafted in Switzerland and Germany. Later, during the late 15th century to the 19th century, France and Switzerland developed artificial limbs that were able to bend and rotate using cables, gears, and springs. However, they still required manual operation through external tools such as cranks. Since the 20th century, manufacturers have been substituting wood and leather for artificial materials such as plastics.

Today, prosthetic devices are primarily made of lightweight and durable materials such as plastic, aluminum, titanium, and silicone, which more closely mimic real limbs. Scientists are developing robotics, 3D printing, artificial intelligence, virtual reality, and motion-sensing technologies for prosthetics. In recent years, researchers have been experimenting with transmitting brain signals through implanted electrodes in an individual’s muscles to move prosthetic limbs more naturally. Currently undergoing clinical trials, the LUKE arm is the world’s most advanced “neuroprosthesis,” an artificial upper arm and hand capable of being controlled by the user’s thoughts through a direct nerve interface directly connected to the user’s nervous system. The LUKE arm, currently designed for trans-radial amputees who have lost their arm below the elbow, enables a “more life-like sensation, increased dexterity, and more intuitive control” (University of Utah, 2025).
Tissue engineering is a technique used to bioengineer living cells and biomaterials to grow tissues to replace or repair damaged or diseased organs—like bones—in the body. To grow bone tissue, cells are typically obtained from stem cells or differentiated cells. Then, they are cultured in bone scaffolds designed to mimic the structure and properties of natural bone tissue and serve as a temporary framework for new bone growth. Scaffolds such as biodegradable polymers or natural extracellular matrices provide mechanical support and structure to the growing cells and guide their growth in a specific direction These scaffolds are typically created from biocompatible materials like ceramics, polymers, or a combination of both, and each material is chosen for its properties in strength, biodegradability, and the ability to facilitate cell adhesion and growth. 3D printing uses precise layer-by-layer deposition, allowing for the creation of complex, patient-specific geometries, mimicking natural bone structure
Bioresorbable Polymers, such as polylactic acid (PLA) and golyglycolic acid (PGA), are biocompatible temporary implants like scaffolds, gradually dissolving overtime within the body, providing support during tissue regeneration, while eliminating the need for removal surgeries
Hydrogels, 3D-printable materials that consist of water-swollen polymers, resemble the natural extracellular matrix that gives support to cells within tissues and organs within the body, making them suitable for cell encapsulation and promoting cell growth. They are used for 3D printing bionics, which can create complex structures for applications like organ-on-a-chip, wound healing, and drug delivery systems.
Bioceramics, used in 3D printing for bone implants and scaffolds, provide excellent biocompatibility and mechanical properties that mimic natural bone, including its porosity such as calcium phosphate-based ceramics like hydroxyapatite.
3D printing allows for the precise customization of bone scaffolds based on the patient's specific anatomical needs. The digital design can be tailored to match the size, shape, and structure of the defect or missing bone, ensuring a better fit and alignment. Furthermore, it enables the fabrication of highly intricate and complex structures that mimic the natural architecture of bone. This includes the incorporation of porous structures, interconnected channels, and specific surface features, which can facilitate cell attachment, nutrient diffusion, and vascularization. 3D-printed bone scaffolds can be made from biocompatible materials, such as bioceramics or biodegradable polymers, that are well-tolerated by the body. These materials promote cell attachment, proliferation, and differentiation, facilitating the regeneration of new bone tissue.
The evolution of orthopedic medicine—from ancient prosthetics to cutting-edge 3D-printed bioresorbable and biocompatible prosthetics—has shown humanity’s continuous struggle against physical ailments. Through the pursuit of the restoration of mobility, humanity has created innovations and techniques that offer solutions to millions of people afflicted with fractures and limb loss.
Citations:
“Amputation and the American Civil War.” Britannica,
Accessed 2 July 2025.
kobah, kylao. “‘my Body’ Series # 3: - The Skeleton: The Framework on Which the Body Is
Built.” First Delta American Hospital, 13 Aug. 2023, fdahospital.org/my-body-series-3-the-
skeleton-the-framework -on-which-the-body-is-built/.
GBD 2019 Fracture Collaborators. "Global, Regional, and National Burden of Bone Fractures in
204 Countries and Territories, 1990–2019: A Systematic Analysis from the Global Burden of
Disease Study 2019." The Lancet Healthy Longevity, vol. 2, no. 9, 2021, pp. e580–e592.
Pike C, Birnbaum HG, Schiller M, Sharma H, Burge R, Edgell ET. Direct and indirect costs of
non-vertebral fracture patients with osteoporosis in the US. PharmacoEconomics 2010;
28: 395–409. 5
Borgström F, Karlsson L, Ortsäter G, et al. Fragility fractures in Europe: burden,
management and opportunities. Arch Osteoporos 2020; 15: 59. 6
Tatangelo G, Watts J, Lim K, et al. The cost of osteoporosis, osteopenia, and associated
fractures in Australia in 2017. J Bone Miner Res 2019; 34: 616–25.
NIH. (2023, May 11). Prosthetics through the ages. NIH MedlinePlus Magazine; NIH.



Comments